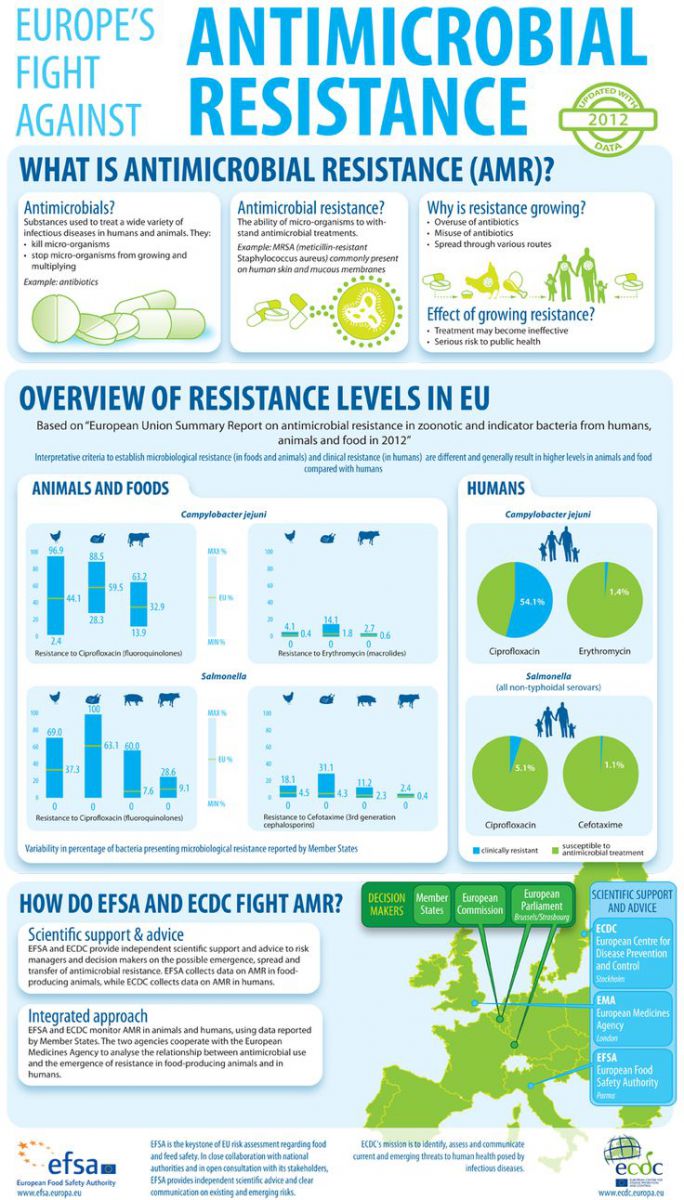
“A problem so serious that it threatens the achievements of modern medicine”. This is how the World Health Organisation describes antimicrobial resistance in its publication Antimicrobial Resistance: global report on surveillance 2014, which came out last month.
They also pointed out that “microorganisms resistant to antimicrobials that emerge in animals may spread to human populations.”
They added “A post-antibiotic era – in which common infections and minor injuries can kill – far from being an apocalyptic fantasy, is instead a very real possibility for the 21st Century.”
Antibiotics have been hailed as one of the great advances in modern health care. Antibiotics (which are also known as antimicrobials, from microbes) are used in human and veterinary medicine to treat infections caused by bacteria. Resistance “is an inevitable consequence of antimicrobials use both in animals and humans” according to the EFSA (European Food Safety Authority).
In Europe, compared to the US, the rules are stricter for conventional food and the use of antibiotics – the last of the growth promotion antibiotics in the EU were officially phased out in 2006. Nevertheless, the authorities, both the EFSA and the ECDC (European Centre for Disease Control) are still concerned with antimicrobial resistance, as can be seen by the extensive data available here.
As they pointed out in a joint statement in March 2014: “Bacteria most frequently causing food-borne infections, such as Salmonella and Campylobacter, show significant resistance to common antimicrobials”
The organisations continue “if bacteria become clinically resistant to several antimicrobials (multidrug-resistant), treating the infections they cause can become more difficult or even impossible. In addition, the development of antimicrobial resistance (AMR) in bacteria in animals and food can also compromise the effective treatment of human infections, as resistant bacteria and resistance genes may be transferred to humans from animals and food. “That’s why a prudent use of antibiotics is crucial, not only in humans, but also in animals”, warned Marta Hugas, Acting Head of EFSA’s Risk Assessment and Scientific Assistance Department.”
Of the farm animals studied, resistance to commonly used drugs was “frequently detected” in broilers, pigs and turkeys. Resistance to critically important drug ciprofloxacin was also high, but resistance to other important antimicrobials was either not detected or reported at very low levels.
For Campylobacter, the results were, if anything, more concerning still. Clinical resistance to common antimicrobials was frequently detected and almost half of campylobacter isolates were resistant to critically important drug ciprofloxacin. EFSA noted that “increasing trends [were] observed in several Member States.” Resistance to commonly used drugs was also frequently detected in animals tested.”
Professor Dame Sally Davies, Chief Medical Officer for England, pointed out that “action is required not only in the area of human health but also animal and agricultural health as 70% of antibiotics worldwide are used in animals.” She also pointed out that “We have reached a critical point and must act now on a global scale to slow down Antimicrobial Resistance. In Europe, 25,000 people a year already die from infections which are resistant to our drugs of last resort.”
So what to do about this? Belgian authorities have instigated an initiative aimed at limiting the use of antibiotics in livestock. There a ten-point plan was launched, to “be implemented by farmers, vets, drugmakers and government agencies” according to agra-net.com. The plan has been developed by the Centre of Expertise on Antimicrobial Consumption and Resistance in Animals (AMCRA), and will aim for a 50% reduction in antibiotics by 2020. As we reported here recently, there are strict restrictions on the use of antibiotics in organic farming, which are even stricter in the US organic farming rules.
More
Great set of infographics on antibiotics.
Arc2020.eu’s dedicated section on antibiotics.